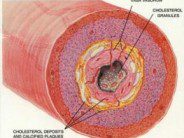
 Osteoarthritis results in the joints due to the mechanical wear and tear of the articular cartilage. Over time, repetitive use and trauma causes the degenerative joint disease to progress by destruction of the cartilage that serves as a shock absorber for the joints of the body. Symptoms of osteoarthritis include joint pain, stiffness, locking, deformity, and decreased range of motion. As the cartilage within a joint becomes thinner, the bones of the joint may come into closer proximity, and eventually touch one another. When the bones of a joint touch one another, the osteoarthritic process can become very painful and immobility can result. The treatment of osteoarthritis usually involves the use of non-steroidal anti-inflammatory (NSAID) medications, which help to decrease pain and inflammation due to cartilage destruction and joint space narrowing. In severe osteoarthritis, NSAIDs fail to provide relief from the symptoms of the disease and surgical intervention is needed. The two most common orthopaedic surgeries that are performed are total knee replacement (TKR) and total hip replacement (THR) surgeries. It is estimated that 1.8 million knee and hip replacement surgeries are performed each year throughout the world.
Osteoarthritis results in the joints due to the mechanical wear and tear of the articular cartilage. Over time, repetitive use and trauma causes the degenerative joint disease to progress by destruction of the cartilage that serves as a shock absorber for the joints of the body. Symptoms of osteoarthritis include joint pain, stiffness, locking, deformity, and decreased range of motion. As the cartilage within a joint becomes thinner, the bones of the joint may come into closer proximity, and eventually touch one another. When the bones of a joint touch one another, the osteoarthritic process can become very painful and immobility can result. The treatment of osteoarthritis usually involves the use of non-steroidal anti-inflammatory (NSAID) medications, which help to decrease pain and inflammation due to cartilage destruction and joint space narrowing. In severe osteoarthritis, NSAIDs fail to provide relief from the symptoms of the disease and surgical intervention is needed. The two most common orthopaedic surgeries that are performed are total knee replacement (TKR) and total hip replacement (THR) surgeries. It is estimated that 1.8 million knee and hip replacement surgeries are performed each year throughout the world.
Researchers, lead by Dr. Arief Lalmohamed of Utrecht University in the Netherlands, have found that the risk of a heart attack is significantly increased after both knee and hip replacement surgery performed for the treatment of osteoarthritis. The results of their study were published online ahead of print in the journal Archives of Internal Medicine. The study was designed as a retrospective nationwide cohort study within the Danish national registries. The study included 95,227 patients who underwent TKR or THR surgery from 1998 through 2007. The investigators followed the study participants post- operatively for the occurrence acute myocardial infarction (AMI, heart attack). Study participants were matched to controls by age, sex, and geographic region. It was found that those over the age of 60 years had increased risk of heart attack after TKR or THR surgeries, and this association was greatest for those over 80 years of age. One in 200 individuals who had a hip replacement had a heart attack, and one in 500 individuals who had a knee replacement had a heart attack within six weeks after the surgery. When compared to individuals of the same age and sex, those who had hip replacement were 25 times more likely to have a heart attack and the risk remained for six weeks after the surgery. Those who had a knee replacement were 30 times more likely to have a heart attack and their risk remained for two weeks after the surgery. The researchers also found that heart attack within one year was a risk factor for post operative heart attack and suggested that elective procedures be postponed till after the risk had decreased.
The authors wrote, “To our knowledge, this is the first study that found that THR (25-fold) and TKR patients (31-fold) are at increased risk of AMI during the first 2 weeks after surgery. The elevated risk was sustained for 6 weeks after THR and for 2 weeks after TKR. The effect of surgery on AMI risk was strongest in patients 80 years or older. The relationship was not more pronounced in those with well known risk factors of AMI (such as heart failure, cerebrovascular disease, and previous AMI), although they increased the risk of AMI within THR and TKR patients. Finally, our data suggest that elective THR surgery should be contraindicated in patients with a previous AMI in the last 12 months before surgery”. In an accompanying editorial, Dr. Arthur Wallace wrote, “The present study once again confirms that the perioperative period increases cardiac risk. Physicians must go further than establishing risk factors; physicians must actively work to reduce perioperative risk… Physicians must carefully review perioperative medications and ensure they are appropriately managed in this critical perioperative period of high cardiac risk. It is important for physicians caring for patients in the perioperative period to recognize the potential for cardiac morbidity and mortality and then appropriately use the armamentarium of medical therapies we now have to reduce cardiac risk, prevent perioperative MIs, and prevent cardiac deaths”.
Traditional risk factors for heart attack have included high blood pressure, diabetes, high cholesterol, smoking, and a family history of early heart attack. Given the findings from this study, controlling risk factors for heart attack during the perioperative period should be a priority. This study also identifies those patients over the age of 60 years, and especially those over the age of 80 years, as the ones with the most risk for post- operative heart attack. In addition, this study gives us a time frame when the risk of post operative heart attack is the highest. Treatment and monitoring for heart attack should be increased for those patients that are at increased risk. Controlling diabetes and high blood pressure, encouraging smoking cessation, and using perioperative beta blockers should be part of the medical management of these patients. Future studies should identify other ways of decreasing the post- operative risk of heart attack for these patients.
Reference:
Arief Lalmohamed et al. “Timing of Acute Myocardial Infarction in Patients Undergoing Total Hip and Knee Replacement” Arch Intern Med 2012;():1-7. doi:10.1001/archinternmed.2012.2713
Image: wikipedia






 DrSamGirgis.com is a blog about medicine, nutrition, health, wellness, and breaking medical news. At DrSamGirgis.com, the goal is to provide a forum for discussion on health and wellness topics and to provide the latest medical research findings and breaking medical news commentary.
DrSamGirgis.com is a blog about medicine, nutrition, health, wellness, and breaking medical news. At DrSamGirgis.com, the goal is to provide a forum for discussion on health and wellness topics and to provide the latest medical research findings and breaking medical news commentary.
{ 0 comments… add one now }