DrSamGirgis.com has the pleasure of hosting the following post by guest blogger, Dr. Richard Andraws MD, who is a Board Certified Cardiologist
According to the most recent figures from the American Heart Association, cardiovascular disease (CVD) accounts for 1 out of every 3 deaths in the United States. CVD is an umbrella term that includes heart attack and stroke as well as other related illnesses. But the first two are by far the most common and feared and are very costly both to their victims and the healthcare system.
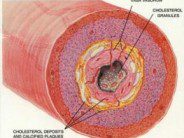
The major risk factors for CVD are pretty well known: high blood pressure, high cholesterol, smoking, diabetes. Many if not most Americans intuitively know that the mantras of “lose weight,” “exercise,” “lower that bad cholesterol” are all focused on heart attack and stroke prevention. Although more than 90% of CVD can be attributed to these traditional risk factors, they may not explain everything. A unifying concept is that inflammation causes CVD. When you think of inflammation, the first images that probably come to mind are redness and swelling and pain. It’s a basic process by which the body reacts to injury or infection and heals itself: an army of white blood cells and proteins on the march against foreign incursion. Sometimes the process is counterproductive and harmful. When it occurs in the lining of blood vessels exposed to high blood pressures, poorly-controlled blood sugars and cholesterol, it ultimately leads to vascular disease, heart attack, and stroke.
What about that last 10%? Since the mid-1990s, a lingering hypothesis has held that infectious agents (e.g. bacteria and viruses) might be the surprising culprits. It makes sense: they’re masters of inciting inflammation, and CVD is, on a basic level an inflammatory process. Bacterial and viral proteins have been found in diseased vessels, strengthening the association. Recently, Kuo and Fujise reviewed data from the National Health and Nutrition Examination Survey, a cross-sectional research database administered by the Centers for Disease Control and Prevention. The investigators analyzed data on more than 2000 women aged 20-59 who were tested for infection with the human papillomavirus (HPV). Of the total cohort, 47% were infected; 60 women self-identified as having CVD (i.e. being told by a doctor that they had a heart attack or stroke in the past). After adjusting for traditional risk factors, women who were HPV positive were almost 3 times more likely to have CVD. Interestingly, only those virus strains associated with cervical cancer were associated with CVD. The authors theorize that the cancer-causing viruses may also affect vascular health by inactivating “tumor-suppressor” genes.
As the authors point out, the retrospective nature of the study, defining CVD by patient recall, and the lack of male subjects, as well as other limitations, make this study hypothesis generating and not definitive. Assuming there is a link between HPV and CVD, what can we do about it? Another bug may just tell us: Chlamydia pneumoniae, a bacterium that commonly causes respiratory tract infections and pneumonia, has also been strongly associated with CVD. An immense amount of research was brought to bear on it in the late 1990s and early 2000s. Several large randomized trials (enrolling approximately 20,000 patients) were conducted to see whether antibiotics could “cure” CVD by eradicating the bacterium. A meta-analysis of these trials conducted by myself and colleagues was, unfortunately, negative; apparently, we couldn’t cure heart attacks with Z-Pak’s. But perhaps we had missed the boat. Once infected, there appears to be no way back because Chlamydia is hard to eradicate and re-infection is common.
With HPV, we have a vaccine. And maybe therein lies the key. An ounce of prevention is worth a pound of cure, as the adage goes. In this case, a simple vaccination could help stem the tide of a CVD menace that kills one American every 39 seconds.
FURTHER READING:
Kuo, HK, Fujise K. Human papillomavirus and cardiovascular disease among U.S. women in the National Health and Nutrition Examination Survey, 2003-2006. J Am Coll Cardiol 2011; 58: 2001-2006.
Heart Disease and Stroke Statistics –2011 Update: A Report from the American Heart Association. Circulation 2011, 123:e18-e209.
Yusuf S, Hawken S, Ounpuu S, for the INTERHEART Study Investigators. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 2004; 364:937-52.
Andraws R, Berger JS, Brown DL. Effects of antibiotic therapy on outcomes of patients with coronary artery disease: a meta-analysis of randomized controlled trials. JAMA 2005; 293:2641-7.






 DrSamGirgis.com is a blog about medicine, nutrition, health, wellness, and breaking medical news. At DrSamGirgis.com, the goal is to provide a forum for discussion on health and wellness topics and to provide the latest medical research findings and breaking medical news commentary.
DrSamGirgis.com is a blog about medicine, nutrition, health, wellness, and breaking medical news. At DrSamGirgis.com, the goal is to provide a forum for discussion on health and wellness topics and to provide the latest medical research findings and breaking medical news commentary.
{ 0 comments… add one now }