DrSamGirgis.com has the pleasure of hosting the following post by guest blogger, Dr. Richard Andraws MD, who is a Board Certified Cardiologist
The more alternatives, the more difficult the choice.
–Abbe D’Allainval
The mainstay blood thinner of the last half century was discovered in spoiled clover that caused cows to bleed to death and subsequently graduated to rat poison before entering clinical use. There is no doubt that warfarin (known by the trade name Coumadin, among others) is an effective anticoagulant. Among patients with atrial fibrillation (AF), it is superior to aspirin at preventing stroke, the arrhythmia’s most feared complication. With an aging and increasingly longer lived population, the prevalence of AF is exploding and with it the need for blood thinning. But warfarin comes with unfortunate baggage: the need for regular bloodwork to monitor effectiveness, frequent dose adjustments, drug interactions, bleeding and significant dietary changes. The last is due to the fact that warfarin inhibits the production of vitamin K-dependent clotting factors; thus, any food rich in vitamin K (and the list is pretty substantial) counteracts it.
Despite all that, warfarin was the only pill in town until recently. In the last year, dabigatran (also known as Pradaxa), became the first FDA-approved alternative. Two other drugs (rivaroxaban and apixaban) are jockeying for position right behind it with two more in the pipeline. After 50 years of pining for an end to warfarin’s tyranny, physicians suddenly have more choices than they dreamed possible. So how do they work? And what distinguishes one from the other?
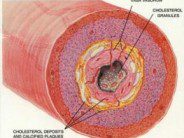
The new blood thinners target the central players in clot formation: Factor Xa (pronounced ten-ay) and thrombin. For baseball aficionados, Xa can be thought of as the starter and thrombin as the closer. They appear to be equally effective targets, and they do not depend on vitamin K for production. Thus, the Xa and thrombin inhibitors require no regular bloodwork and dose adjustments and no dietary modifications, a huge plus for patients. They do require good compliance, however, as their effects dwindle quickly after each dose; so missing one or two doses can be dangerous. Warfarin in comparison stays in the bloodstream for much longer once therapeutic.
In the beginning, there was the thrombin inhibitor dabigatran. Based on the RE-LY trial, the FDA approved the drug to prevent stroke in AF not due to valvular heart disease. RE-LY enrolled 18,000 patients with AF and risk factors for stroke and compared two doses of dabigatran (150 mg and 110 mg twice daily) to warfarin. The investigators wanted to prove dabigatran was just as good (i.e. noninferior) to warfarin, but surprisingly, the higher dose proved superior in preventing strokes and other embolism and death due to vascular causes. Dabigatran also caused less brain hemorrhages, but appeared to cause more bleeding from the gastrointestinal tract (in fact, Australian regulatory authorities just issued a warning regarding this). Bleeding was related to age and illness. Thus, for those at higher bleeding risk, and particularly those with impaired kidney function (the kidneys clear the drug from the bloodstream), the FDA approved a 75 mg dose, but not the 110 mg dose. There is no evidence on how effective this dose is.
Rivaroxaban, a Xa inhibitor, made its debut soon after dabigatran was approved via the ROCKET-AF trial. Similar to RE-LY, this was a large trial of 14,000 AF patients in which once a day rivaroxaban was compared to warfarin. Unlike dabigatran in RE-LY, rivaroxaban was not superior to warfarin at preventing stroke, but appeared to be just as good. Similar to dabigatran, rivaroxaban caused less brain hemorrhage, but there was no excess gastrointestinal bleeding. A controversial issue is whether rivaroxaban was “fairly” compared to warfarin. Because warfarin needs to be constantly adjusted, a patient may spend a certain portion of the time with “low” levels and therefore not be effectively anticoagulated. In ROCKET-AF, patients in the warfarin arm were therapeutic only 58% of the time (less than other trials). So maybe rivaroxaban looked better than it really is. More analyses are forthcoming.
Then, in the twilight of the Parisian summer, apixaban, another Xa inhibitor, burst onto the scene at the European Society of Cardiology’s Congress. The ARISTOTLE trial of 18,000 AF patients compared twice daily apixaban to warfarin. As with dabigatran, apixaban was superior to warfarin at preventing stroke and embolism. It caused no excess bleeding and significantly reduced death from all causes.
So where do we stand? Thus far, only dabigatran is approved in the United States. Rivaroxaban and apixaban will soon be considered for approval by the FDA. Assuming all three come to market, clinicians will likely have to tailor their choice carefully. For a patient having compliance problems, perhaps once-daily rivaroxaban would make the most sense. Would a patient at higher risk for bleeding do better on the untested 75 mg dose of dabigatran or twice daily apixaban? Does apixaban’s all-cause mortality benefit trump all? And for valvular AF patients, the whole debate is, unfortunately, moot.
Sometimes, an embarrassment of riches is just that. But more often than not, having options is good for patients as well as their doctors.
REFERENCES:
Roderick LM. A problem in the coagulation of the blood; sweet clover disease of the cattle. Am J Physiol 1931; 96: 413–6.
Stahmann MA, Huebner CF, Link KP . Studies on the hemorrhagic sweet clover disease. V. Identification and synthesis of the hemorrhagic agent. J Biol Chem 1941; 138 (2): 513–27.
Weitz JI. Factor Xa or thrombin: is thrombin a better target? J Thromb Haemost. 2007 Jul;5 Suppl 1:65-7.
Dabigatran versus Warfarin in Patients with Atrial Fibrillation (Available at: http://www.nejm.org/doi/full/10.1056/NEJMoa0905561)
Rivaroxaban versus Warfarin in Nonvalvular Atrial Fibrillation (Available at: http://www.nejm.org/doi/full/10.1056/NEJMoa1009638)
Apixaban versus Warfarin in Patients with Atrial Fibrillation (Available at: http://www.nejm.org/doi/full/10.1056/NEJMoa1107039)
Dabigatran (Pradaxa): risk of bleeding relating to use (Avaialble at URL: http://www.tga.gov.au/safety/alerts-medicine-dabigatran-111005.htm)






 DrSamGirgis.com is a blog about medicine, nutrition, health, wellness, and breaking medical news. At DrSamGirgis.com, the goal is to provide a forum for discussion on health and wellness topics and to provide the latest medical research findings and breaking medical news commentary.
DrSamGirgis.com is a blog about medicine, nutrition, health, wellness, and breaking medical news. At DrSamGirgis.com, the goal is to provide a forum for discussion on health and wellness topics and to provide the latest medical research findings and breaking medical news commentary.
{ 1 comment… read it below or add one }
Brain hemorrhage is of course deadly, you need your head to be examined as soon as possible if you think that you have hit your head hard. ,”`”.
Kind thanks